The skull isn’t meant to be opened, but sometimes it has to be
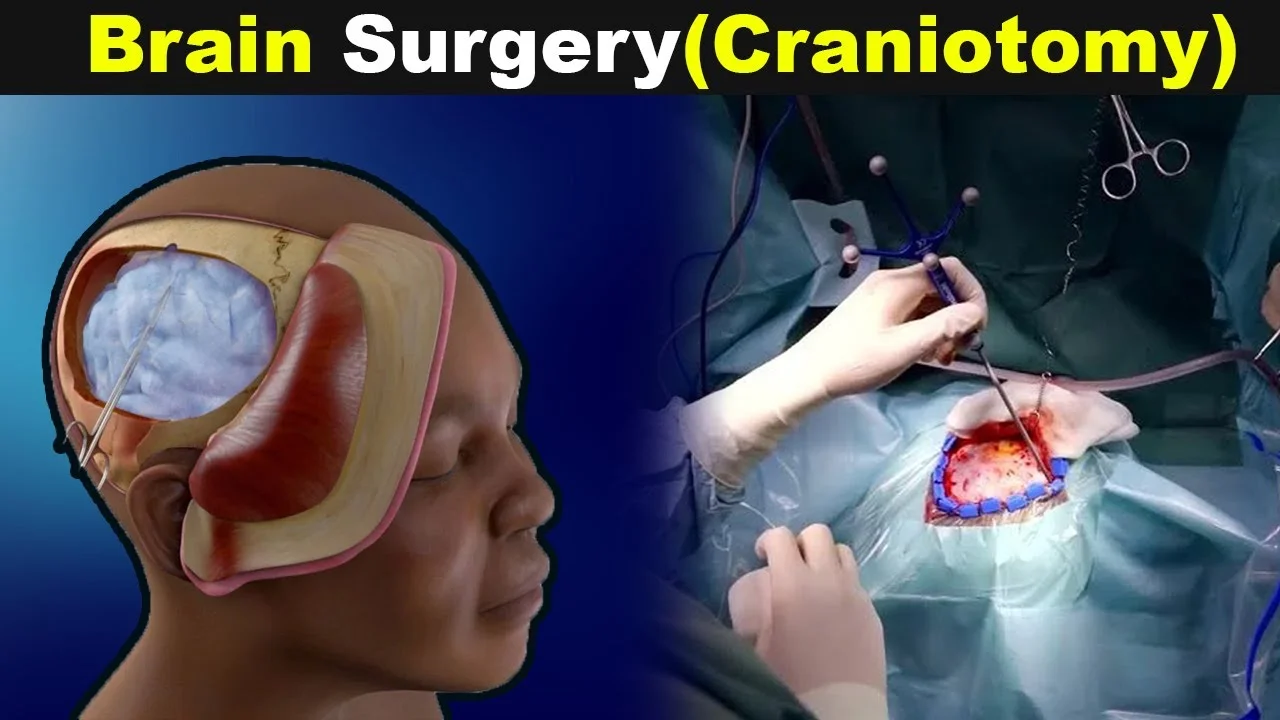
A craniotomy begins where most things shouldn’t. With a cut to the head. A window in the skull. Bone temporarily removed. The brain, exposed. It sounds extreme. Because it is. But for some, it’s the only way forward. The only way in. The only way out.
It’s not done without cause. It’s never routine. But sometimes, nothing else works. Blood pools. Tumors grow. Pressure builds. And the only solution lies behind the bone. That’s when the decision is made.
It’s done to reach what can’t be touched any other way
Brain surgery doesn’t begin with wires or scopes. It begins with space. Surgeons need a way in. The skull doesn’t flex. So they make an opening. It’s precise. It’s planned. But it’s still invasive.
Craniotomy gives access to remove tumors. Clip aneurysms. Drain bleeding. Remove clots. Sometimes it’s to implant electrodes. Other times, to remove infections. It’s a tool—not a treatment itself, but a way to treat.
Not every craniotomy is the same
Some are small. Others large. Some happen while you’re asleep. Others while you’re awake. Yes, awake. Because the brain can’t feel pain. And staying conscious helps surgeons protect what matters—speech, memory, movement.
Sometimes the bone is replaced right away. Other times, it’s stored. Inside the body or in a freezer. To be reattached later. When swelling settles. When danger has passed.
Preparation takes longer than the surgery itself
Scans come first. CT. MRI. Angiograms. They map everything. Not just where to cut, but what to avoid. Blood vessels. Nerves. Critical regions.
Then comes planning. Positioning. Anesthesia. Monitoring. Craniotomy doesn’t happen in a rush. Even emergencies follow steps. One mistake is too many. The brain leaves no room for error.
Recovery isn’t just physical
The incision heals. The bone reattaches. But the brain needs time. It swells. It slows. It rewires. Some people lose words. Others lose balance. Or memory. Or sight. These may return. Or they may not.
Fatigue lasts weeks. Sometimes longer. Mood changes. Concentration dips. Not because of the cut—but because the brain was touched. Moved. Disrupted. And it remembers.
The risks are as serious as the reasons
Infection. Bleeding. Stroke. Seizures. These risks are real. And they’re explained in detail. Because consent isn’t just about permission. It’s about knowing what’s at stake.
But not doing it carries risks too. Leaving a tumor untouched. Letting pressure build. Ignoring bleeding. Sometimes, the risk of not opening the skull is worse than the risk of doing so.
It’s not the end of the journey, just the beginning
Craniotomy doesn’t fix everything instantly. It’s a step. Often the first. Followed by therapy. Medications. Check-ups. Scans. Rest. Life slows down after brain surgery. It has to.
Work waits. Conversations take more effort. Light feels brighter. Sounds sharper. You learn what your brain needs. And what it doesn’t tolerate anymore.
Emotions shift in unexpected ways
Some feel relief. Others feel grief. Even when surgery goes well. Something changes. A sense of fragility. Of awareness. That your brain has been touched. And that stays with you.
Depression is common. So is anxiety. It’s not weakness. It’s healing. The brain recovers at its own pace. And sometimes, it mourns before it mends.
Craniotomy sounds violent, but it’s careful
This isn’t reckless. It’s deliberate. Millimeter by millimeter. Guided by maps, tools, hands that have trained for years. It’s not loud. Not rushed. Not dramatic like the movies.
But it is serious. Because the brain is serious. And when something threatens it, the skull becomes a door. One that only opens when there’s no other way.
