It begins with something that doesn’t feel quite right
A headache that stays too long. A word that won’t come. A hand that shakes without reason. Not always painful. Not always dramatic. Just strange. And it lingers. That’s how many brain tumors first show up. Quiet. Subtle. Easy to ignore.
It could be pressure. It could be swelling. Sometimes it’s confusion. Sometimes vision. Nothing loud. Nothing obvious. But the brain notices before you do. And that’s when testing begins.
Not every tumor means cancer
The word tumor sounds final. But it isn’t always. Some tumors are benign. They grow slowly. Stay contained. Don’t spread. But they still press on the brain. That pressure can shift everything—speech, memory, balance.
Malignant tumors act differently. They grow fast. They move. They return. And they don’t always stay where they started. But even then, not all hope disappears. Treatment exists. Even when the name is hard to hear.
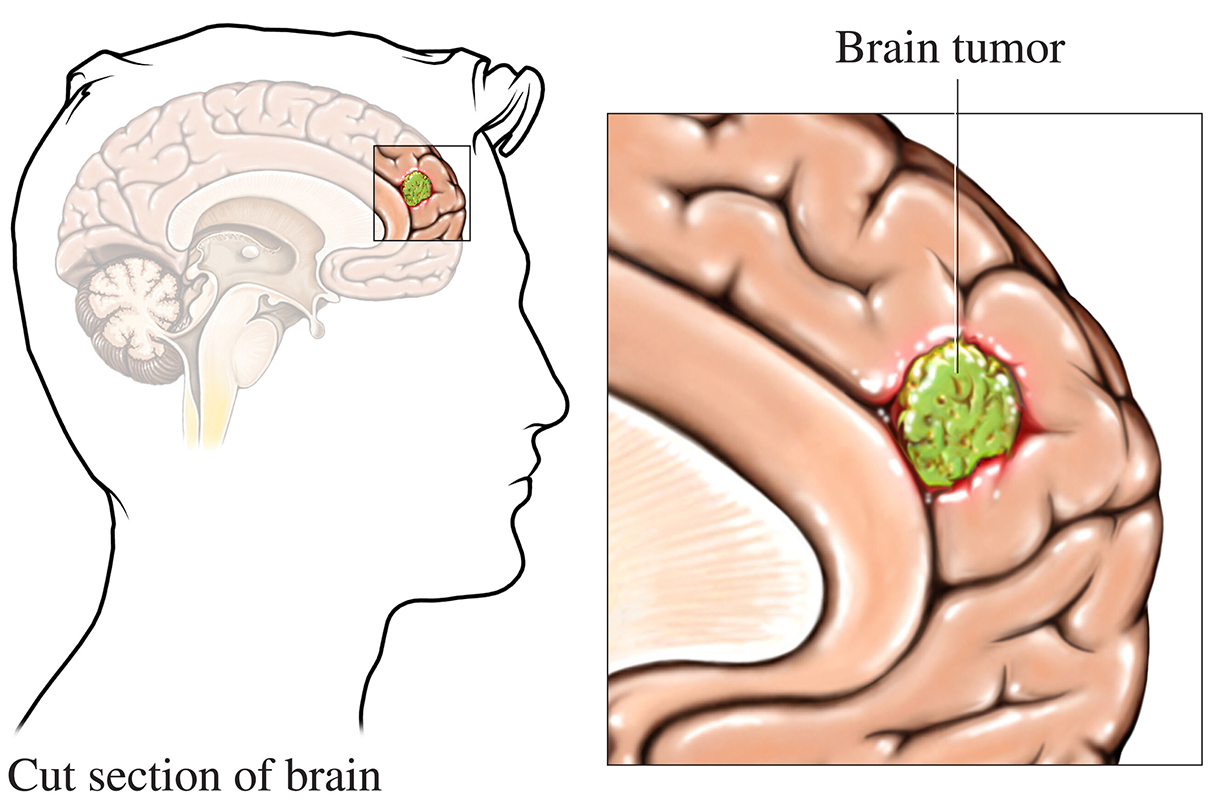
Where it begins makes all the difference
Primary brain tumors start in the brain. Gliomas. Meningiomas. Pituitary tumors. Each type behaves differently. Grows in different places. Affects different functions.
Secondary tumors start elsewhere. The lung. The breast. The skin. They travel through the blood. And settle in the brain. These are metastatic. But they are still treatable. Sometimes with radiation. Sometimes with surgery. Sometimes both.
Gliomas behave based on the cells they come from
Astrocytomas grow from star-shaped cells. Some stay slow. Others change quickly. Oligodendrogliomas come from support cells. Often slower. More responsive to treatment. Ependymomas block fluid. That causes swelling. Pressure. Headaches.
Glioblastomas are the most aggressive. Fast-growing. Hard to remove completely. But they’re not untreatable. They just require more—more time, more therapy, more care.
Meningiomas don’t always need surgery
They grow from the brain’s lining. Not the brain itself. Often benign. Often slow. Some are never removed. Just watched. Scanned every few months. If they grow or cause symptoms, then action follows.
Others grow silently. Then press on nerves. Cause seizures. Vision changes. Then removal becomes necessary. But it depends on size. On location. On the person.
Pituitary tumors change hormones before anything else
They don’t usually cause pain. But they change energy. Weight. Mood. Fertility. That’s because they affect hormone production. Too much. Too little. And everything feels off.
They’re often found during hormone tests. Or scans for unrelated reasons. Some shrink with medication. Others need surgery. But most are manageable once found.
Symptoms depend on where the tumor sits
A tumor near the speech center affects words. Near the motor cortex, it affects movement. Near the optic nerves, it affects sight. The brain works in regions. And tumors press where they land.
That’s why symptoms are so different. The same tumor in a different spot would feel like something else entirely. There’s no single pattern. Just signs that don’t add up.
Diagnosis is more than just a scan
MRI is usually the first tool. Sometimes CT. Sometimes both. But diagnosis also needs exams. Questions. Reflex checks. Eye tracking. Balance testing. Every clue matters.
Sometimes a biopsy is needed. A piece of the tumor, tested in a lab. To see what cells are inside. That’s how doctors choose treatment. The name matters. But so does the behavior.
Treatment depends on more than the tumor
Age matters. Health matters. Location matters. Some tumors can’t be reached easily. Others sit near critical areas. Surgery becomes risky. Or impossible. Then other treatments take the lead.
Radiation shrinks tumors over time. Chemotherapy targets them with drugs. Newer options use the immune system. Some people get all of them. Others only need one. The plan is never the same twice.
Surgery removes what’s possible, but not always everything
The brain is delicate. So is a tumor’s location. Surgeons remove what they can. Without harming too much. That’s the goal. Balance. Safety. Precision.
Sometimes they leave part of it. On purpose. To protect speech. Or movement. That’s where radiation helps next. It targets what’s left behind. Slowly. Over weeks.
Radiation comes in different forms
External beams are most common. Focused. Daily sessions. Over days or weeks. Other times, radiation comes from inside. Tiny seeds. Or wires. Placed during surgery.
Stereotactic radiosurgery sounds like surgery, but isn’t. It’s a single, high-dose beam. Very precise. Often used for small tumors. Or those deep inside.
Chemotherapy crosses the barrier with difficulty
The brain protects itself. That’s good. But it makes chemo harder. Not all drugs can enter. Some are designed to cross. Others are given directly into the spine. Or during surgery.
Side effects vary. Fatigue. Nausea. Hair loss. But not always. Newer drugs target cells more precisely. The goal is always the same—slow growth, shrink size, buy time.
Immunotherapy is still growing
It uses the immune system. Teaches it to recognize cancer cells. To attack them. Like it would a virus. It works for some tumors. Not all. Trials are ongoing. Hope is growing.
It doesn’t replace other treatments. Yet. But it adds to the options. Especially for those with few choices left. Especially when nothing else works.
Living after treatment feels different
Even when the tumor is gone, recovery continues. Words may come slower. Fatigue may linger. Scans become part of life. So do follow-ups. And sometimes, fear.
But many return to work. To family. To daily life. It just takes time. And patience. And support. Not just from doctors. But from people who stay close.
